ACLU and DRRI Urge RI TO Shift Funding For Children's Mental Health
/By Gina Macris
Disability Rights Rhode Island (DRRI) and the American Civil Liberties Union of Rhode Island (ACLU) made an urgent plea May 24 to the House leadership to shift its focus on residential treatment for acute children’s behavioral health issues to “robust funding” for comprehensive community-based services accessible at home and at school.
The letter to Joseph Sheckarchi, Speaker of the House; Majority Leader Christopher Blazejewski, and Finance Committee Chairman Marvin Abney, comes on the heels of federal findings that the state harms children in prolonged institutional care, - and in the midst of the General Assembly’s final negotiations on the upcoming state budget.
The timing gives the General Assembly an opportunity for “righting the current course and establishing a long-term solution for children rather than continuing on its apparent present course of spending tens of millions of dollars on residential treatment facilities,” wrote Morna Murray, executive director of DDRI; and Steve Brown, executive director of the ACLU.
They said the cost of residential settings is “astronomical” compared to the costs of serving children in the community.
According to the federal findings released last week, the state spent more than $13.6 million in Medicaid dollars on psychiatric hospitalization of children in state care between July 1, 2020 and June 30, 2021 and nearly $27 million for children’s residential treatment during the same period – some of it out of state.
In-state residential treatment can cost as much as $990 a day, while therapeutic foster care may cost $48 to $125 a day, U.S. Attorney Zachary Cunha said in a complaint alleging the state for years has violated the civil rights of children with behavioral health issues.
Meanwhile, the state budget proposal that would take effect in about five weeks – on July 1 - contains $11 million to expand the troubled St. Mary’s Home in North Providence, even though the state’s child welfare agency is pulling children out of that facility.
In addition, the state is planning to spend $45 million over the next three years to build an intensive residential treatment facility for girls in Exeter, on the site of the former Ladd School, which once housed people with intellectual and developmental disabilities.
Last week’s DOJ findings warned about the harmful effects of long-term hospitalization and institutional care on children. It serves as a “wake-up call” that the state “cannot build its way out of its obligations to care for vulnerable youth in the state,” said Brown in a statement.
“This long-standing issue harms the most vulnerable children and represents a violation of their legal rights,” said Murray in the same statement. “The time has come for the state to comprehensively correct this injustice,” she said.
Quoting the U.S. Attorney, Murray and Brown said in the letter that “it’s not an issue of not enough beds.”
Study after study has shown that children treated during long stays in hospitals and psychiatric residential facilities, like St. Mary’s Home for Children, experience physical and emotional abuse, over-medication, trauma and rehospitalization at higher rates, with their long-term success in life diminished, the letter said.
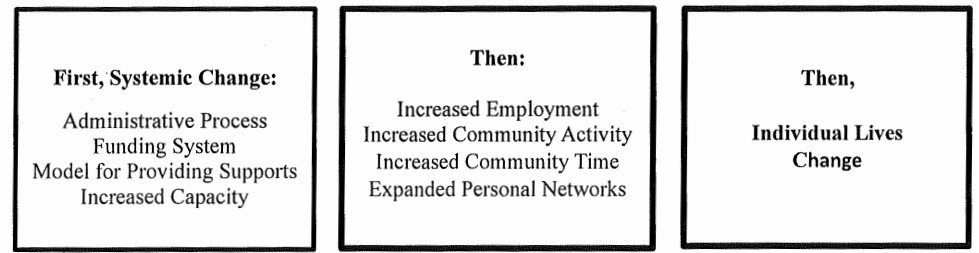
Brown and Murray asked the House leadership to take the DOJ findings to heart and to re-direct into the community the funding which put more children in residential treatment facilities “that cannot solve the problem.”
Companion bills sponsored by Sen. Louis DiPalma, chairman of the Senate Finance Committee, and Rep. Tina Spears, D-Charlestown, Westerly, South Kingstown and New Shoreham, would require the General Assembly to fully fund rate increases for a broad array of home and community services as recommended by the Office of the Health Commissioner (OHIC) every two years.
The governor’s budget would spread out existing OHIC recommendations over the next three years, with $22.1 million proposed for the next fiscal year.
Future rate reviews would be conducted once every four years for each of four categories for community services, according to a budget amendment the governor submitted to the General Assembly in April.
Developmental Disability News asked spokespersons for both the governor and the House leadership on May 23 – a day before the DRRI and ACLU letter - whether the DOJ complaint will affect budget talks about the OHIC-recommended increases for the next fiscal year, but there has been no immediate response from either.
May 23 was the deadline for the state to respond to the DOJ complaint, which alleged that the state violated the Integration Mandate of the Americans With Disabilities Act (ADA) by “warehousing” children with behavioral problems at Bradley Hospital, the state’s only children’s psychiatric hospital.
DCYF director Ashley Deckert wrote to Assistant U.S, Attorney Amy Romero May 22, saying “we look forward to working cooperatively with the U.S. Attorney’s Office and HHS (the Department of Health and Human Services) to address the findings.”
Deckert said she will call Romero “shortly to establish a framework for our collaboration going forward” to find a “mutually agreeable strategy to address what we believe are nationwide mental health staffing challenges.”