RI DD Services Get A "Status Quo" Budget, But Can It Keep Up With Client Needs And Consent Decree?
/By Gina Macris
With Rhode Island Governor Gina Raimondo signing the $9.6 billion budget bill into law June 22, the service system for adults with developmental disabilities averts a crisis in the fiscal year beginning July 1, and instead continues the status quo.
That is to say, the system is still struggling to meet the needs of some 4,000 Rhode Island adults with developmental disabilities, including those who are seeking services for the first time.
Higher-than-expected revenue estimates in May enabled the House and the Senate to restore a number of reductions in the human services which Raimondo had proposed in January, including about $18 million in developmental disabilities. On June 20, the Senate ratified the House version of the budget and sent it to the governor.
Until the state’s intent to restore the funds for developmental disability services became clear in mid-May, an independent federal court monitor had been preparing to make recommendations to U.S. District Court Judge John J. McConnell, Jr. for an order to ensure adequate funding..
It was the second time since a federal civil rights consent decree was signed in 2014 that a court order, or the threat of one, has surfaced during the budget-making season at the State House. There’s no reason to believe that the monitor won’t re-visit that idea next year if funding for developmental disability services fails to keep pace with the stepped-up demands of the consent decree, which requires the state to shift from segregated services to those offering integrated, community-based opportunities by 2024.
One goal illustrates the challenges. The state is to have part-time jobs by Sept. 30 for all young adults who left high school between 2013 and 2016 and who who want to work, but with three months remaining until the deadline, those with jobs number 235, or 55 percent, of a population of 425, according to figures released last week.
The budget does include $1.5 million in technical assistance for private providers of developmental disability services trying to adjust to integrated services for clients, according to Carmela Corte, the chief financial officer of the state Department of Behavioral Healthcare, Developmental Disabilities and Hospitals (BHDDH). Those are federal-state Medicaid dollars that will be taken from the allocation for direct services.
A relatively small number of adults with developmental disabilities who choose to use their funding authorizations from BHDDH for in-home care will be able to pay workers 10 percent more, which amounts to about $620,000 in the budget, Corte said.
By The Numbers
The General Assembly also adjusted the current budget to close out the fiscal year, adding about $15.6 million to cover an operating deficit as recommended by Raimondo, who acknowledged the shortfall deficit as a one-time event.
The overall numbers in developmental disabilities:
- $272.1 million for Fiscal 2018, which ends June 30
- · $271.4 million for Fiscal 2019, which begins July 1
Administrators, however, tend to work on a day-to-day basis with an “operating budget,” which includes only federal and state Medicaid funds available for providing direct services.
For the current fiscal year, federal-state Medicaid dollars are budgeted at $269.8 million. For the fiscal year beginning July 1, the federal-state Medicaid total is $269.2 million.
No Raises For Frontline Workers
One big-ticket item missing from the next budget is a pay increase for employees of private service providers who work directly with adults with developmental disabilities. The underpaid workforce is sure to be a major issue for advocates when the General Assembly reconvenes in January.
Incremental raises for these workers during three budget cycles have allowed them to keep just ahead of the minimum wage, in a range which puts private service providers in competition with the same pool of workers as fast-food restaurants and other retail businesses.
Including the most recent raises, in 2017, the average direct care worker is paid about $11.50 an hour. The minimum wage, which increased from $9.60 to $10.10 on Jan. 1, is due for another bump, to $10.50, on Jan. 1, 2019.
Before the General Assembly cut $26 million from the developmental disabilities budget in 2011, the average pay at some private agencies serving adults with developmental disabilities averaged close to $15 an hour, with comprehensive health insurance and other benefits. Career ladders afforded front-line workers opportunities for advancement.
Since then, the workforce has become unstable, with employers unable to fill one out of six jobs, according to the Community Provider Network of Rhode Island, a trade organization. Turnover ranges from about 30 percent to about 75 percent, depending on the agency. In some cases, workers leave direct care work for other jobs with similar pay but much less responsibility. In other cases, they leave for the same type of work at better pay in Massachusetts, which is scheduled to offer a minimum of $15 an hour for such work July 1.
Budget Questions At Public Forum
The issue of worker pay surfaced at a public forum hosted by the Division of Developmental Disabilities (DDD) June 18 at the University of Rhode Island, with one parent lamenting the lack raises in the year ahead.
Kerri Zanchi Photo By Anne Peters
Kerri Zanchi, Director of Developmental Disabilities, and other staff of the Department of Behavioral Healthcare, Developmental Disabilities and Hospitals (BHDDH), explained various aspects of the budget and outlined initiatives intended to help the service system in the long run.
Asked whether the “status quo” funding approved by the General Assembly would result in cost overruns in the coming fiscal year, Zanchi didn’t say. Instead she emphasized that DDD must use its data “every single month” to support its projections and “really understand what our needs are going to look like.”
But BHDDH projections of need for developmental disability services don’t figure in the semi-annual Caseload Estimating Conference that comes up with figures for Medicaid entitlement costs.
And the state Budget Office does not take actual costs into account in making recommendations to the governor, a spokeswoman said earlier this year. Rather it uses “estimated growth rates in the cost of providing services,” according to Brenna McCabe. She did not say who makes the estimates or otherwise elaborate.
The new budget doesn’t allow for increases in individual funding authorizations – one of the chief causes of the cost overruns which prompted the BHDDH request for additional funding in the budget cycle now winding down.
The governor cited higher “acuity” in acknowledging that increased per-person costs fueled a projected $15 million deficit in developmental disability costs in the fiscal year ending June 30. That factor, however, was ignored in her presentation of Fiscal 2019 budget that begins July 1.
Ever since November, 2016, there has been an upward trend in individual authorizations, something that is expected to continue for several years, until all clients have been evaluated at least once using a revised standardized interview that is considered more accurate than the previous one. Both the original interview, called the Supports Intensity Scale (SIS), and the revised one, called the SIS-A, were developed by the American Association on Intellectual and Developmental Disabilities.
Budget Language Opens Door To Innovation
The budget contains language that responds in to a variety of concerns about who manages resources available to adults with developmental disabilities and how providers are paid.
It gives BHDDH the required state legislative authority to apply for a so-called “Health Home” and an “Alternate Payment Method” to create pilot programs for changes in case management and provider reimbursement better suited to integrated, community-based services that are tailored to individual preferences and needs, as required by the Americans With Disabilities Act.
The Centers for Medicare and Medicaid Services (CMS) hold that neither the states, as funding authorities, nor the services providers themselves can also be responsible for designing and managing individualized programs of activities without conflicts of interests.
States should have another disinterested party in the role of case manager, according to CMS.
The Health Home is the CMS name for the third-party case management organization that would oversee individual clients’ Medicaid and Medicare services, while the Alternate Payment Method allows states to explore changes to the usual fee-for-service reimbursement to private providers.
Zanchi and Kimberly Reynolds, BHDDH administrator of financial management, explained the goals of the applications at the public forum June 18.
Reynolds described the Health Home as a “one-stop shop where individuals and families may get assistance in managing their services. BHDDH has three health homes, mostly in the substance abuse and mental health areas.”
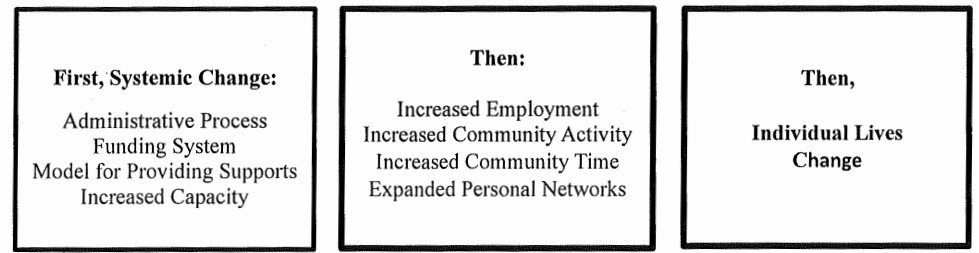
By way of background, Zanchi said that the idea for applying for a Health Home grew out of collective thinking in DDD during the last year about ways to put its clients in the driver’s seat in shaping their activities, or as she put it, developing “person-centered practice.”
For one thing, the system can’t be truly “person-centered” without case management that is free of conflicts of interest, Zanchi said.
She also said a pilot program for an Alternate Payment Method might generate solutions to problems faced by the current fee-for-service reimbursement system, which poses challenges to providers trying to get their clients into the community in meaningful ways.
The fee-for service system requires providers to bill in 15-minute increments, but only when a client is actually receiving services. It doesn’t allow providers to plan ahead, because reimbursement depends on day-to-day attendance at a particular activity, without exceptions for occasions such as client’s medical appointments, illnesses, or vacations.
As the state moves to a system with greater consumer control and consumer empowerment, Zanchi said, providers will need to be able to count on more staff to get their clients into the community.
Despite the consent decree, the reimbursement system is still geared to funding programs held in facilities like sheltered workshops and day centers, where one staff member can keep an eye on larger groups of individuals than is possible in the community.
Zanchi and Reynolds each said they want the public to participate in drawing up the applications for the Health Home and Alternate Payment Method.
“We have a lot of work to do in a very quick time frame, and like everything else we’ve done, we’re going to do it with our constituents,” Zanchi said.
The state anticipates submitting the applications, receiving decisions, and beginning pilot programs by next Jan. 1, according to Zanchi. CMS would pay 90 cents on the dollar to support the pilot programs for a maximum of two years.
Flyers distributed at the meeting gave a schedule for public meetings on the applications, but the schedule was put on hold. Reynolds said she is the contact person for the Health Home. She can be reached at 401-462-3941 or at Kimberly.Reynolds@bhddh.ri.gov