RI DD Funding System Harms Quality Of Life, Advocates Tell House Finance Subcommittee
/By Gina Macris
Anxiety, frustration, and fear permeate the lives of adults facing the daily challenges of developmental disabilities, and by extension, the lives of families and caregivers who support them, say numerous Rhode Islanders who wrote to members of the House Finance Committee recently to explain the human effects of chronically underfunded services.
“The person receiving support grieves and is forced to live in a state of perpetual frustration” because of missed opportunities resulting from staff shortages, wrote Diane Scott, who has worked 29 years at West Bay Residential Services. Likewise, “the impact on employee morale is a palpable anxiety and frustration,” Scott said.
Howard Cohen * Photo by Anne Peters
Jacob Cohen has had to begin taking a “significant regimen of medication to control his anxiety so he could deal with his daily life,” wrote his parents, Howard and Patricia Cohen of North Kingstown. They said it has been “heartbreaking” to watch him lose control of his daily activities as funding has shrunk over the last decade.
The letters from Scott, the Cohens, and others served as written testimony in a March 28 budget hearing on the state Department of Behavioral Healthcare, Developmental Disabilities and Hospitals (BHDDH) before the House Finance Subcommittee on Human Services, chaired by Rep. Alex Marszalkowski, D-Cumberland.
And some of concerns expressed before the finance subcommittee about the quality of care overlapped with remarks made a few hours earlier the same day before a special legislative commission studying the state’s fee-for-service reimbursement system for private developmental disability services, Project Sustainability.
Another letter writer, Holly Walker said she knows a client of AccessPointRI who spends every Monday morning telling everyone how upset she is that she missed Sunday church services – again – because there was no one available to take her.G
A Warwick mother, Pam Goes, wrote that frequent change of staff has increased her own fears about the safety of her non-verbal son.
“Staff who don’t know him struggle to know what he needs, at home and in the community. He is unable to tell them when he is sick, when something hurts, when he is afraid. And my fears are increased as well,” Goes wrote.
Two other mothers, Lisa Rego and Claudia Swiader, asked members of the Finance Committee “to put themselves in the shoes of the parents and families of individuals with a developmental disability.”
“Wouldn’t you want to know that your loved one was being cared for by someone who wanted to be there? Wouldn’t you want to know that your loved one was receiving the support they needed to keep them safe, healthy and happy?” wrote Rego and Swiader, president and vice president, respectively, of the Autism Society of Rhode Island.
Scott, the veteran caregiver at West Bay Residential Services, reminded legislators that “any Rhode Island citizen may be one injury or disease away from needing support for a disability.”
The children and families of workers also suffer the consequences of inadequate funding, others said.
Brandi Ekwegh of Cumberland, a former manager of an AccessPoint group home and a single parent, described missing her tween-aged daughter’s concerts and award ceremonies and even leaving her home alone at 2 a.m. because there was no one else to de-escalate a client’s behavioral outburst at work.
When her daughter said she spent more time with her clients than with her, Ekwegh said, “I was crushed but she was absolutely correct.”
Disabled Have Civil Right To Services
By any measure, caring for adults with developmental disabilities is costly, but the integration mandate of the Americans With Disabilities Act also entitles them to services that allow them to access their communities for competitive employment and leisure activities of their own choosing.
The currently enacted budget for the state Division of Developmental Disabilities (DDD) totals $271.7 million in federal and state Medicaid money and miscellaneous other funds. Governor Gina Raimondo would add another $9.2 million to that bottom line, for an overall $280.9 million, to erase an existing deficit and pay for services during the fiscal year beginning July 1.
About $1.6 million in savings taken from the state-operated group home system, Rhode Island Community Living and Supports, would boost funding for privately-run services by $11 million over the next 15 months, according to information presented by the House Fiscal Office.
Within the $11 million total increase, Raimondo would set aside $6.4 million in Medicaid funds, including $3 million in state revenue, to raise the wages of front-line developmental disability staff by an estimated 34 to 41 cents an hour, depending on who’s drafting the projection.
Providers, Families, Seek $28.5 Million For Wages
Many of the letter-writers urged the Finance Committee to hike the state’s commitment for wages to $28.5 million, so that employers can meet unfunded overhead expenses in addition to passing along a wage increase to all their employees. Every Medicaid dollar the state spends generates a little more than a dollar in the federal Medicaid match.
As it now stands, the governor’s proposed increase would apply only to front-line workers, who typically make roughly $1 to $2 above minimum wage, if that.
In a letter to Marszalkowski , the subcommittee chairman, Kevin McHale, an administrator at AccessPoint, wrote that the average direct care worker at his agency makes $10.77 an hour, only slightly above minimum wage.
McHale, once a direct care worker himself, recalled that in 1987, the General Assembly voted to make a “substantial investment” in the private provider system by raising the pay of direct care workers to $7 an hour, about 90 percent above minimum wage, which was then $3.65 an hour.
At a time when the state was preparing to close the Ladd School, its only institution for persons with developmental disabilities, “this investment was seen as an intentional statement on the importance and value of the vital and challenging (yet rewarding) work that direct support professionals perform,” McHale wrote.
Today, private service providers operate at a loss for each person they employ, they say.
Regina C. Hayes, executive director of Spurwink RI, provided the committee with tables showing that the state funds a fulltime direct care position at $34,454, including an allowance of 35 percent of wages for employee-related expenses. But that figure is almost $9,900 per-person less than what it costs Spurwink for mandatory taxes, vacation, sick and holiday pay and health insurance, Hayes said.
The percentage the state pays for employee-related overhead is set through “Project Sustainability,” the controversial fee-for-service system enacted by the General Assembly in 2011.
Howard and Patricia Cohen, Jacob’s parents, say that Project Sustainability has harmed their son. The change in reimbursement methods “masqueraded as an improvement but in effect was merely a way to reduce costs,” they wrote.
Those already receiving services are not the only ones affected by the budget constraints.
Agencies Can’t Afford New Clients
Linda Ward, executive director of Opportunities Unlimited, a service provider, said that current funding and staffing situation makes it difficult for her agency to take on new clients or launch new initiatives.
Opportunities Unlimited recently had to “step back” from plans to develop a home designed to meet the significant psychiatric and behavioral needs of four women, Ward said.
Her testimony echoed comments made earlier in the day by Gloria Quinn, executive director of West Bay Residential Services, who addressed the special legislative commission studying Project Sustainability.
Families of young people aging out of the special education system often struggle to find agencies that are able to provide services for their sons or daughters, she said.
“We can’t find the staff”, said Quinn, a commission member. An agency’s ability to respond to the demands of the community is at its heart “a wage issue,” she said.
Andrew McQuaide, a senior director at the Perspectives Corporation, called the situation “self-directed by default,” meaning that parents who may not otherwise chose to do so are left to manage their loved ones’ individual programs because they can’t find an agency to provide appropriate services.
McQuaide, another member of the Project Sustainability commission, said that so-called self-directed families are having the same problems as the agencies in hiring direct care workers, but the families are doing it “without support.”
At the commission meeting, Barbara Burns said she recently decided to do a self-directed program of day services for her sister, not because she wants to do it but because it was the only way she could get respite care. Burns’ sister has Down syndrome and Alzheimer’s disease and lives with her on Aquidneck Island.
A proposal in the governor’s budget would create an “independent provider” model of care through the Executive Office of Human Services with a single fiscal intermediary to give those needing services at home broader choice in selecting caregivers.
The independent provider model also would give BHDDH the option selecting one fiscal agent to manage the accounts of self-directed families of adults with developmental disabilities, Linda Haley, a House fiscal advisor, told the finance subcommittee.
The prospect of unwanted change has worried some families, but a BHDDH spokesman said April 1 that DDD will continue with five fiscal intermediaries in accordance with its regulations, as well as a desire to give consumers choice.
Burns, meanwhile, said there should be a single state bureaucracy to address the needs of people with developmental disabilities, whether they are children in school, healthy adults, or people facing chronic illness or the end of life. Families face enough challenges caring for a special child, she said.
Semonelli * image courtesy of capitol tv
Christopher Semonelli, vice president of Rhode Island Families Organized for Change and Empowerment (RIFORCE) , made the same point to the finance committee’s human services subcommittee a few hours later.
Parents of special education students describe the transition to adult services as “falling off a cliff,” said A. Anthony Antosh, Director of the Sherlock Center on Disabilities at Rhode Island College.
Rebecca Boss, the BHDDH director, told commission members that there are other ways to increase wages for direct care workers besides adding to the bottom line.
Even if the state increased wages, Boss said, the milennials millennials making up the current entry-level workforce are “a little different.” Direct care workers need adequate training and supports. “It’s about making sure people love their jobs,” Boss said.
L to R: Louis DiPalma, Rebecca Boss, Heather Mincey OF DDD. * Photo By Anne Peters
Wages are “part of it,” she said, but “I’m hesitant to say it’s the solution. It’s part of the solution.”
She recalled testimony presented to the commission in January about Vermont’s system, which included higher rates for direct care workers but much less reliance than Rhode Island on costly group homes.
Later, Boss told the House Finance subcommittee that she wants to reduce the number of adults with developmental disabilities living in group homes from the current 32 percent to the national average, 26 percent.
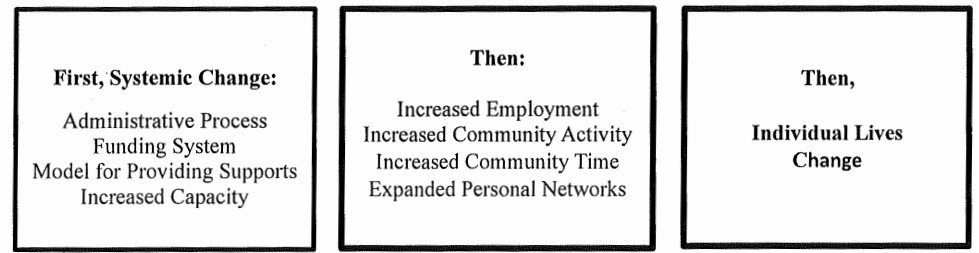
BHDDH also has launched a review of the reimbursement rates the state pays to private providers under the terms of Project Sustainability, with an eye toward creating an alternate payment model to the current fee-for service system.
Tom Kane, CEO of AccessPoint, reminded the finance committee members that the same healthcare consultant who helped develop Project Sustainability has just recommended that California increase developmental disability budget by 40 percent, or $1.8 billion. Rhode Island should be prepared for a a report that recommends a similar percentage increase, ane said, given that the state underfunded Project Sustainability from its inception.
Louis DiPalma, D-Middletown, the chairman of the Project Sustainability commission, made the same point earlier in the day.
The consultant hired for the rate review and study of alternate payment model, Elena Nicolella, executive director of the New England States Consortium Systems Organization, will speak at the next meeting of the Project Sustainability commission, according to DiPalma, the commission chairman. Nicolella is also a former Medicaid director in Rhode Island. The date of that meeting has not yet been set.