Pandemic Pushes Worry Over RI DD System Survival “Front And Center” - Judge McConnell
/By Gina Macris
Judge McConnell
The federal judge overseeing the reform of Rhode Island’s developmental disability system says the COVID-19 pandemic has sharpened his concern about the financial ability of the state and its service providers to meet long-term goals of the consent decree, which mandates integration of the target population at work and at play.
Other participants in a May 18 hearing in U.S. District Court in Providence echoed the judge’s concerns, but they also said the pandemic has created a great opportunity to cement changes that might not otherwise have come as quickly.
“The fiscal health and stability of providers has always been in the back of my mind,” said Chief Judge John J. McConnell Jr., noting that his worry has come “front and center with this crisis.” Stability is “essential for the consent decree to play out and be seen as accomplished,” he said.
The state and federal governments in 2014 agreed to a civil rights consent decree mandating employment-related services to provide access to jobs in the community for people with developmental disabilities as well as supports to allow them to enjoy integrated non-work activities. The decree runs until 2024.
Kevin Savage
During the hearing, Kevin Savage, the state’s new Director of the Division of Developmental Disabilities, disclosed immediate financial concerns. He said that the state has not received approval from the Centers for Medicare and Medicaid Services for the second of three advance payments promised to keep private providers fiscally afloat during the height of the pandemic.
On March 26, the state Department of Behavioral Healthcare, Developmental Disabilities and Hospitals (BHDDH) announced that a total of $15.4 million in federal-state Medicaid funding had been set aside for these so-called “retainer payments” during April, May, and June.
While the April payment has received CMS approval, the one for May has not, Savage said. A BHDDH spokesman later said that $5.1 million in advance payments to providers were made May 15.
Savage said it was “important that the state make that payment” to the providers.
The BHDDH spokesman later elaborated:
“When the retainer payments were first described and provided in Rhode Island, CMS had not issued technical guidance on these types of payments.” Since then, he said, CMS has limited retainer payments to a 30-day period, but that “the state is actively working with CMS to expand this time frame.”
CMS reimburses a little more than half of any Medicaid cost applied to the Division of Developmental Disabilities, but if the federal government ultimately does not approve the May 15 payment to providers, the state will be responsible for the entire $5.1 million.
As to the June advance payment, Savage said during the court hearing that the money will be re-cast as an increase in Medicaid rates that adds up to the same amount originally promised to providers.
He also disclosed that one provider decided to change the type of services it offers and the executive director resigned over the issue. Going forward, Savage said, he understands that particular agency would be “less focused” on the kind of individualized work his division wants to do, but he reserved further comment until he has had a chance to speak in depth with agency officials.
The hearing was streamed via the internet application Zoom, as have been previous U.S. District Court proceedings since the federal court building on Kennedy Plaza was closed in early March at the start of the pandemic. For the first time on May 18, however, the hearing was arranged so that the public could see the participants as well as hear them.
Victoria Thomas, a lawyer for the U.S. Department of Justice, said the DOJ is “very focused” on how those protected by the consent decree will get community-integrated services going forward.
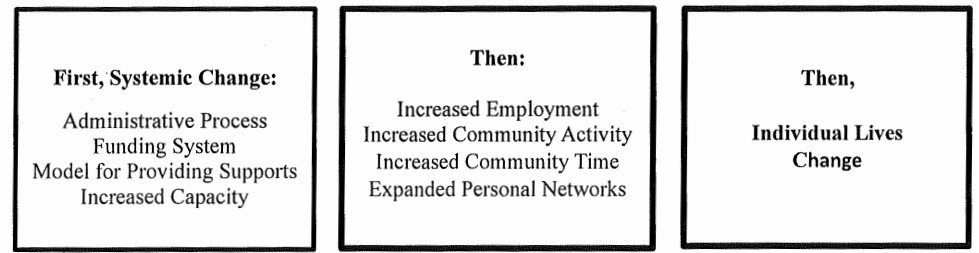
The capacity of providers to deliver those services involves more than funding, she said. The state needs to make administrative changes to ensure a stable system of integrated services and supports.
A. Anthony Antosh, the independent court monitor in the case, pressed for two immediate administrative changes:
● Annual funding authorizations for service recipients to replace the quarterly allocations now in place.
● The end of prescribed staffing ratios according to five funding “tiers,” which are based on perceived levels of disability and do not necessarily reflect the amount of support needed for a task at hand.
Savage said the staffing ratios are written into Medicaid rules, and BHDDH could work administratively with CMS to eliminate them. The ratios were designed for center-based day care and providers have argued that the ratios do not work in an individualized community setting. Families and other advocates also oppose them.
Savage said the quarterly funding authorizations were enacted by the General Assembly and cannot be changed without its approval. The fiscal arm of BHDDH favors quarterly payments, he said.
Melody Lawrence, Director of Policy and Delivery System Reform at the state Executive Office of Health and Human Services, said the argument for quarterly authorizations is to “ensure that the resources go to those who need them most.”
McConnell questioned how often people’s service needs change.
“You are doing more frequent checks to make sure people actually need those services,” Lawrence replied.
Two experts have testified before a special legislative commission that Rhode Island is the only state with quarterly funding of adult developmental disability services, a feature which providers have said repeatedly makes it difficult for them to plan ahead or prepare for the kinds of long-term changes the consent decree demands.
The commission, led by State Sen. Louis DiPalma, D-Middletown, recommended more than a year ago that the state switch to annual funding of individualized service plans. It is generally accepted among developmental disability professionals that barring unexpected events, like the death of a family member, the needs of individuals with intellectual and developmental challenges remain fairly stable and predictable throughout their lives.
Savage said that fiscal officials at BHDDH are committed to creating a funding model that is “easier and more straightforward” for providers and families to navigate.
Thomas, the DOJ lawyer, told Savage: “We’ve been hearing that quarterly authorizations create an administrative burden on providers. We like hearing that you want to reduce administrative burdens.”
McConnell asked Antosh to report to the Court by the end of June what the state has done to ease administrative burdens on providers.
Antosh indicated his report will also include a rundown on the changes the state must undertake to satisfy the consent decree by 2024.
Based on his comments in the hearing, he is likely to include recommendations for increased reimbursement rates to providers and provisions for universal access to internet technology for those receiving developmental disability services.
During the hearing, Antosh asked Savage in the short term to eliminate the scale of rates it pays for various daytime direct support work and instead pay the highest one – assigned to community-based activities - for all front-line staff work.
Savage reminded Antosh of the state’s budget deficit, which has been estimated at $234 million in the fiscal year ending June 30 and a whopping $800 million if the next budget cycle is included in the total. He said his division would start on a case-by-case basis by focusing on funding the needs of each individual authorized to receive supports.
Antosh said a lack of access to internet technology has emerged as a big failing during the pandemic. Group home residents need access to wireless networks, as well as to tablets and other hardware that could help them feel less isolated and in the long run could assist providers with remote wellness checks and the like.
A relative handful of people receiving BHDDH-funded supported employment services have been able to work from home, Antosh said, but more would like to try, according to survey results passed on to him.
Technology must be part of the long-term future for the developmental disabilities service system, he said.
The pandemic has curtailed most daytime services and providers’ ability to bill for them in the current fee-for-service reimbursement system. Most of the daytime activities that have occurred have involved outdoor exercise, Antosh said.
At the same time, providers have had to bear the burden of costly cleaning protocols and other unexpected expenses in group homes that are not automatically reimbursed by the state.
As of Tuesday, May 19, the coronavirus affected 47 congregate care sites, according to the BHDDH spokesman. A total of 115 people in congregate care have tested positive, including 5 who were reported hospitalized on Tuesday. An additional 98 people have been exposed to the virus because of where they live but were asymptomatic. And 7 more persons have died from COVID-19, the spokesman said.
Antosh, meanwhile, said the coronavirus crisis has highlighted the fragility of families as well as providers as they have scrambled to support loved ones with developmental disabilities.
Families often have had no support in caring for adult children or siblings who may need attention of one kind or another all their waking hours – and during the night as well.
Antosh said those who direct their own program of services have had difficulty finding staff to relieve them during the crisis. About 700 persons or families direct their own programs, and BHDDH relaxed its rules on hiring staff to allow any capable adult – including parents and legal guardians who might otherwise be out of work.
Savage said a long-standing prohibition against paying legal guardians to support adults who receive BHDDH funding will not be re-instated after the state of emergency is over.
Antosh said 80 percent of family members answering a questionnaire distributed by a coalition of community organizations reported a high level of anxiety.
Seventy percent said they were concerned about what might happen if their loved one needed to be hospitalized or if they themselves became ill and could not continue as caregivers.
(The state Department of Health recently advised hospitals to make exceptions to their no-visitation policy during the pandemic for those who needed assistance in communications and the support of a familiar caregiver to understand medical procedures.)
Outside BHDDH and the Rhode Island Department of Education, which is responsible for transition services for high school students with developmental disabilities, state officials have been “slow to realize how vulnerable this population is,” Antosh said.
But once they understood, officials in other state agencies have become very sensitive to the needs of those with intellectual and developmental disabilities.
He cited the hazard pay awarded to group home workers, a large order of personal protective equipment (PPE) delivered to providers two weeks ago, and another large order for family caregivers that arrived last week, and an increased focus on testing individuals and staff over the last several weeks.
Antosh said “all parties” have joined in discussions about “what re-opening looks like.”
File photos by Anne Peters